As mentioned in our previous blog, “The Inevitable HCIS Downtime,” your healthcare information system (HCIS), which houses all your patient information, can be brought down for reasons that are planned (maintenance, upgrades, etc.), but unplanned downtimes can occur at any time due to a number of reasons, including a loss of power, network connectivity, natural disaster, or even a system failure. Network, system and power outages occur annually, and always at a cost and impact to your organization.
The Cost of Downtimes
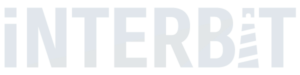
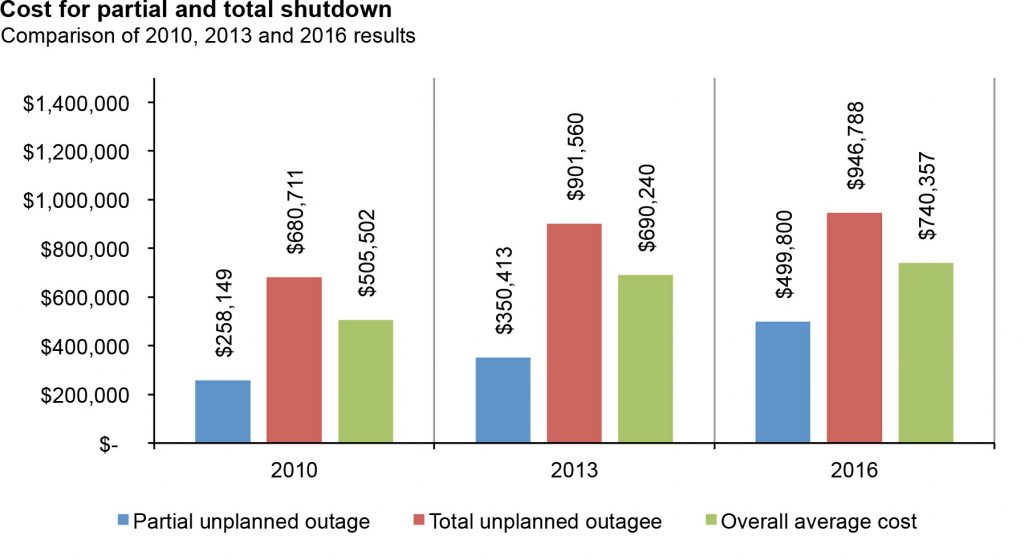
Healthcare facilities face average costs of $740,357 per downtime incident, according to the findings of the 2016 Ponemon Institute study. This is roughly a 38 percent increase over what was reported in 2010. Of course, those numbers depend on several factors, which include the length of the downtime and its complexity, but overall, organizations typically have to shell out over $8,851 per minute of downtime.
“This increase in cost underscores the importance for organizations to make it a priority to minimize the risk of downtime that can potentially cost thousands of dollars per minute,” said Ponemon in the report.
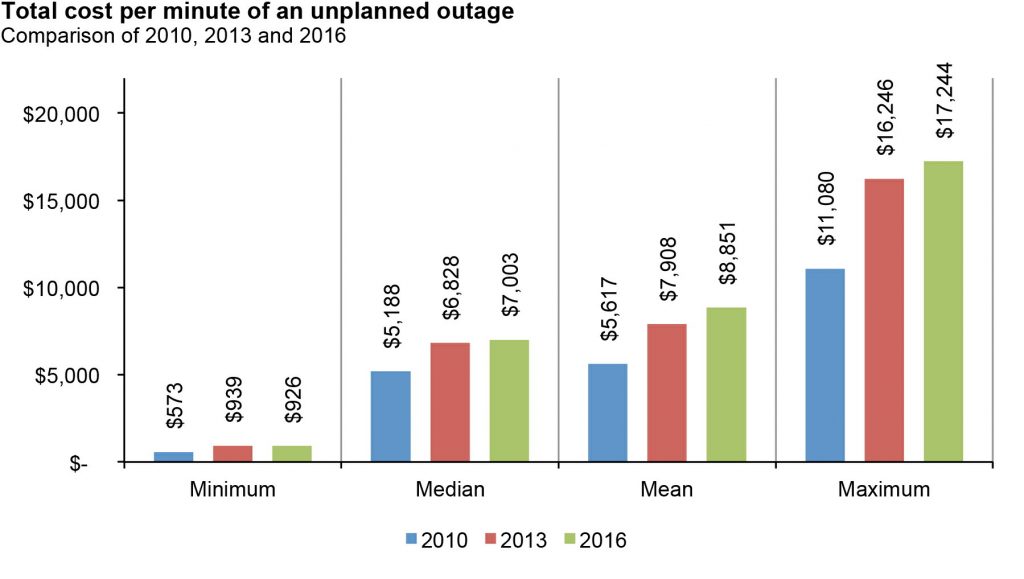
The most significant cost organizations incurred after data center or system outages were business disruption costs, pegged at an average of $256,000; lost revenue costs, averaging $208,600; and end-user productivity, an average of $138,200 lost per incident, according to the 2016 report.
Out of 15 industry sectors covered in the report, healthcare saw the third highest costs, above eCommerce, retail, transportation, consumer products, co-location, services, media, education, and hospitality sectors.
As mentioned in our previous blog, partial downtimes occur more than twice as often as total downtimes. Device-level outages, or those limited to individual servers occur four times as often. Even though many partial downtimes may not be regarded or recorded as a downtime, they can cost half as much.
The Real Impact of Downtimes in Healthcare
When a system downtime occurs in a healthcare facility, the financial costs incurred are really the least of the organization’s concerns. There are serious potential consequences involving patient safety and the delivery of patient care.
When your healthcare information system goes down, your clinicians are not only unable to access the patient information they need — they’re unable to access the most up-to-date information. Changes in patients’ medications and treatments often occur and nurses and other clinicians need to be informed of any new status with a patient. If, for instance, they are not aware that a patient has developed an allergic reaction to a previously-prescribed medication and then administer that med based on an older medication record, the results could be disastrous.
The disruption to patient-specific processes and workflow when a system downtime occurs leads to diminished responsiveness to patients and interruptions in the delivery of patient care. Essentially, your clinicians’ ability to provide quality care is compromised. If they are unable to access the information they need from the healthcare information system to do their jobs and treat their patient, patients will suffer the consequences. Patient satisfaction is critical to your business, as it impacts your HCAHPS scores and the public perceptions and investments that are tied to them. However, a patient fatality that results from slow responsiveness or the use of out-of-date information can cost your organization far more than its reputation and customer service scores.
To find out more and learn how you can reduce the costs and impact of HCIS downtimes, check out our whitepaper, Healthcare Business Continuance: Implementing Procedures to Address Critical System Downtimes.